CASE 2: Robotic assisted primary hip replacement, with post-operative CT to check the 3D implant position
The Story
“Judy, a 69-year-old retired orthopaedic secretary, came to see me with rapidly deteriorating right hip pain. She had been suffering for many years and then, over a period of 6 months, the pain worsened so that she was only able to crawl upstairs once a day.
She had other significant medical problems and was very aware of orthopaedic technologies and outcomes after hip replacement.”
The Investigation
A CT scan was used to plan her Mako robotic hip replacement.
The Evidence
Anteroposterior plain radiograph demonstrating superior destruction of the right acetabulum with bone on bone contact secondary to loss of cartilage.
The Diagnosis
Judy was diagnosed with end stage osteoarthritis of the right hip causing severe impairment to her daily life, requiring operative intervention.
The Plan
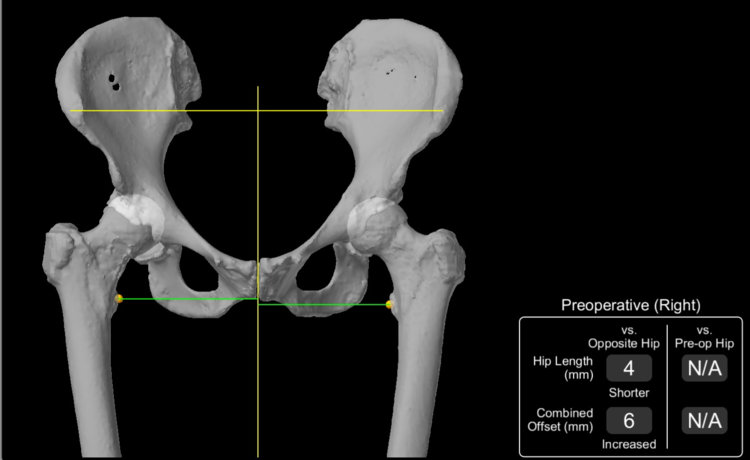
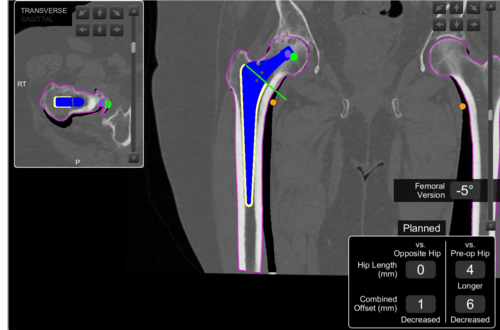
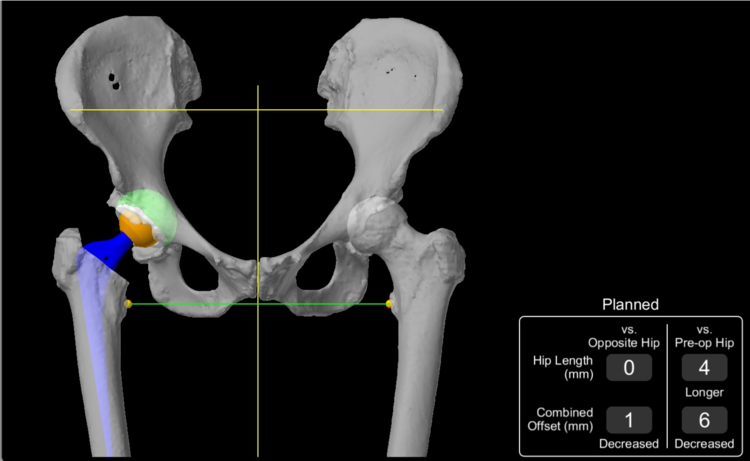
Using software developed by the robot manufacturers, the pre-operative CT scan was used to reconstruct a virtual 3D model of Judy’s hemipelvis. This allowed for the perfect implant size and position to be planed, using accurate measurement tools integrated into the software.
One of the biggest challenges with using robotic guidance is calibrating the machine (the robot) to the hip (the patient). In this process, known as registration, the surgeon maps corresponding points from the virtual 3D model to the patient’s true anatomy intraoperatively, so the robot understands the positioning of the patient and the exact location of different anatomical points.
Planning images from the robotic planning software. Various parameters are calculated by the software to allow for planning the perfect hip replacement.
The Operation
The operation is carried in the usual way with 2 main additions.
First, pins are placed in the iliac crest (top of the pelvic bone) so that the robot knows where the pelvis is at all times. Secondly, the surgeons orientate the robotic arm to the hip joint so that the robotic arm can help the surgeon achieve the plan on the computer screen.
During the operation the robotic arm guides the bone preparation tools and the final position of the implants. The surgeon holds the robotic arm at all times: in other words, the robotic arms simply tweaks the positioning of bone preparation and implant insertion tools.
The Outcome
3D CT analysis is accurate and precise in measuring implant component orientation.
Anteroposterior plain radiograph of the pelvis demonstrating good positioning of the new right sided implant.
Post-op CT of the pelvis demonstrating good positioning of the new right sided implant.
Post-op analysis of the implant position comparing pre- and post-op CT scans showed a near perfect positioning outcome. The femoral lengths demonstrated a 0mm discrepancy, with a 1mm discrepancy in the vertical and horizontal femoral offset.
Judy recovered as normal, walking within 12 hours of surgery and requiring minimal pain killers. The real benefit will come later on: leg length equalisation will allow more normal walking; and implant position will allow confidence with movements and a longer lasting hip implant. The post op CT analysis above showed an almost perfect position of the hip implants.
The Verdict
“The Mako robotic arm adds 10 minutes to the operation but gives the surgeon extra confidence in the accuracy of the position of the hip implants.
The Mako demands a higher level of planning, using a CT scan before the operation, which adds a small cost, some radiation dose and some hassle for the engineers. But if it means starting the operation knowing the implant sizes required and the bony anatomy of the patient, then this is worth it.”
-
Robots have been used in orthopaedics for decades but the Mako is the first to be used on a worldwide basis and has reached the greatest number of surgeons and done the most number of orthopaedic operations when compared to any other robot.
-
-
Compare to the pros and cons of patient specific instrumentation, which also uses CT for planning but instead of a robotic arm it uses 3D printed custom-made guides that fit onto the patients bony anatomy.
Compared to a robot, this involves more hassle pre operatively (due to the 3D printing) but saves time in surgery because the guides are simply placed directly onto the bone and do not have to be registered to the bone by a computer.