CASE 36: Revision for adverse reaction to metal debris (ARMD) using a custom internal proximal femoral replacement
The Story
“Jim was referred to me 8-years after his primary hip replacement. He initially had a large diameter metal on metal hip replacement which survived for 4-years before he suffered significant pain secondary to metallosis. This was revised by his local team to a cemented long femoral stem, which initially performed well.
A few months after the revision, despite a good radiographic appearance of the construct, Jim started to experience significant lateral thigh pain. This progressed over the next three years until the pain become unbearable, at which point he was referred to my care. The pain was so excruciating that on one occasion, it caused him to fall leading to a broken collar bone.
Jim was an otherwise healthy 70-year old gentleman. He enjoyed cycling, walking and badminton, but the pain was preventing him from doing all of this.”
The Investigation
On clinical examination, Jim was in significant pain around his left hip, impacting on his normal activities of daily living. He had a reduced range of all movements in the left hip secondary to pain. He had a positive Trendelenburg test on the left hand side. His Oxford hip score at presentation was 26/48.
As with all painful hip replacements, we performed blood inflammatory markers, which came back as normal.
He was discussed in our metal debris disease MDT. They confirmed that there was evidence of proximal osteolysis in the femoral stem however they felt distally the stem was well fixed.
The Evidence
Anteroposterior plain radiograph showing Jim’s cemented long femoral stem (after revision of a large diameter stemmed MOM hip replacement). This was taken 6-weeks after the revision procedure at his local hospital. Compare this to the images to the left to see how the femur has remodelled around the cement mantle.
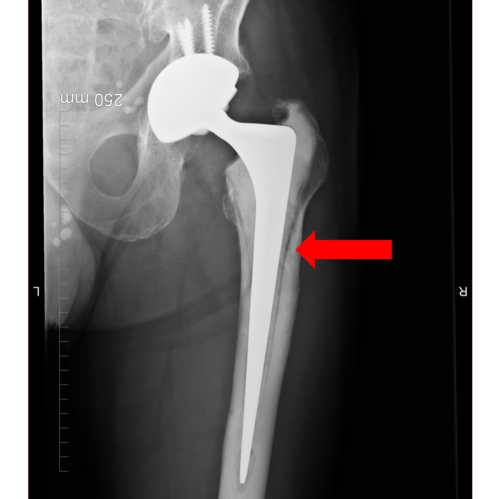
Anteroposterior plain radiograph of Jim’s left proximal femur taken at the time of presentation. This close up image demonstrates the significant osteolysis laterally (red arrow) between the cement mantle and the endocortex of the femur.
Anteroposterior plain radiograph of Jim’s pelvis taken when Jim first presented to me. This radiograph was taken 3-years after Jim’s first revision (as seen on the left) and it demonstrates significant osteolysis surrounding the long cemented stem.
Lateral plain radiograph of Jim’s left proximal femur taken at the time of presentation. There is evidence of osteolysis and fragmentation in the anterior femoral cortex in the subtrochanteric region (white arrow) which continues distally.
The First Diagnosis
Jim was diagnosed with a loose left femoral stem likely secondary to corrosion of the cobalt chrome long femoral stem (metal on metal debris from the bearing increases the chance of corrosion of a CoCr stem below, even when the metal on metal bearing has been removed). This was in the absence of any infection.
The First Plan
The initial plan with Jim was to revise his femoral component to a long modular taper fluted stem while retaining the acetabular component.
The First Re-Revision Operation
We used a posterior approach via the old scar to access the hip. After dissection of the soft tissues, it was obvious that the proximal 15cm of bone and periosteum was dead with a corroded cement mantle. We used an extended trochanteric osteotomy (15cm in length) to remove the old stem and cement mantle.
A large Restoration modular taper fluted stem was cemented in situ with cables used around the proximal bone. A ceramic head was used, with the existing acetabular component retained and the joint was assessed for stability and length. We were happy with the reconstruction, so the surgical site was washed and closed with vicryl and clips.
The First Outcome
Anteroposterior and lateral radiographs taken immediately after Jim’s revision surgery. This shows the extended trochanteric osteotomy with cables surrounding the proximal portion of the long modular taper fluted stem.
Anteroposterior and lateral radiographs taken 8-months after Jim’s first operation demonstrated displacement of the lateral fragment proximal to the osteotomy site with some compression of the osteotomy seen in the lateral radiograph.
At 8-months after the operation, despite promising initial recovery, mobilising on two crutches initially down to one, Jim had a sudden episode of mid-thigh pain. The radiographs taken at this clinic are above. His case was once again discussed at the metal debris disease MDT where the verdict was decided that the bone from the lesser trochanter down to the osteotomy site was likely to be dead, with the rest of the femur being healthy.
The Second Diagnosis
Dead proximal femoral bone (due to metal debris from a corroded stem) with non-union of an extended trochanteric osteotomy with the risk of breakage of the modular taper fluted stem.
The Second Plan
Jim needed a solution that would work for him to get him back on his feet. We decided to use a custom internal proximal femoral replacement which was designed from a CT scan. This allowed us to preserve his native muscle attachments at the trochanters while giving him a stable femoral implant.
Coronal CT used for planning and designing the custom internal proximal femoral replacement.
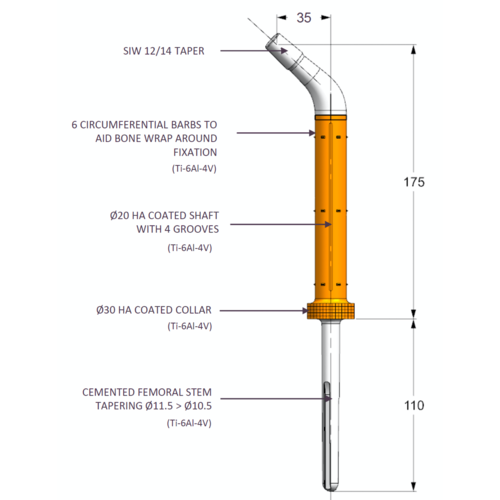
Planning image of the new custom internal proximal femoral replacement. This has been designed using the existing implant as a reference as this was well positioned despite the dead proximal femoral bone. The orange section of the stem represents areas covered in hydroxyapatite to encourage bony ingrowth.
Planning image reconstructed from the coronal CT scan. This image demonstrates the existing femoral stem within the proximal femur. The measurements have been used to work out the length of the custom internal proximal femoral replacement.
Planning image demonstrating the custom femoral stem within the pre-operative femur (reconstructed from the coronal CT). The CT insert within the image is there to demonstrate the footprint of the hydroxyapatite coated collar which has been designed into the stem.
The Second Operation
For the second operation, we used the same posterior approach through the old incision and protected the soft tissues with stay sutures. The cup remained well fixed so was left in situ. We took five samples to send to microbiology to rule out infection. The femur was severely affected, however there was at least 60% good muscle attachment to the proximal portion.
We performed an osteotomy and removed the modular taper fluted stem with ease. The custom internal proximal femoral replacement was cemented in situ and a restricter was used. A 32mm head was used and the length and stability were both good. We secured the remaining proximal femoral bone stock with two cables before washing and closing.
The Second Outcome
Anteroposterior and lateral plain radiographs taken immediately after the implantation of the custom internal proximal femoral replacement.
EOS imagining taken 6-month after Jim’s procedure demonstrates that the custom internal proximal femoral replacement is in a great functional position.
Jim had a complex series of operation to get him to this stage, however when I reviewed him 6-months after the operation, he was doing very well. He was able to walk across my clinic room very well unaided and was only using a single stick to help him with longer distances. He had a full range of pain free movement and was able to stand on one leg. At home he was using a static exercise bike to try and rehabilitate is abductor muscles with great success.
The Verdict
“Metal debris disease from MOM bearings can be difficult to treat. Try to avoid using CoCr cemented stems for revision of these bearings. Suspect ongoing corrosion of the femoral stem if the proximal femoral bone does not heal.”
-
At the London Implant Retrieval Centre (www.lirc.co.uk) in 2016, we reported evidence of severe corrosion of CPT cobalt-chromium (CoCr) hip stems (used in 25,000 people in the UK) that are fixed in bone using cement and are a source of toxic metal ion release and should be removed.
Previously, surgeons would retain the stem to avoid damage during removal: now they are removing these stems.
-
Harry S. Hothi, Reshid Berber, Andreas C. Panagiotopoulos, Robert K. Whittaker, Camilla Rhead, John A. Skinner, Alister J. Hart: Clinical significance of corrosion of cemented femoral stems in metal-on-metal hips: a retrieval study. International Orthopaedics 01/2016; 40(11)., DOI:10.1007/s00264-016-3116-4
-
Please see all our other cases of revision of MOM hip implants.